What is IVF?
IVF (in vitro fertilisation) is a fertility treatment where a sperm fertilises an egg outside the body. “In vitro” literally means “fertilisation in glass” which is why IVF is also called “test tube babies”.
What is IVF?
IVF (in vitro fertilisation) is a fertility treatment where a sperm fertilises an egg outside the body. “In vitro” literally means “fertilisation in glass” which is why IVF is also called “test tube babies”.
Many couples will be advised to consider IVF treatment. During a woman’s normal monthly cycle one egg grows and is released (ovulated). As this happens the fallopian tube moves to collect this microscopic egg. Meanwhile sperm must swim from the vagina, through the cervix and womb into the tube to find the egg. Once beside the egg several sperm must bind to it for one to complete its journey and enter the egg. Specialized microscopic hairs and muscle in the wall of the fallopian tube move the fertilized egg down the tube into the womb as it changes to become an embryo. Once inside the womb the embryo must find a place to implant in the womb lining and become a pregnancy.
If the egg is not fertilized by a sperm her period will start 14 days later. If the Fallopian tubes are blocked or cannot pick up the released egg, then the egg and sperm can’t meet and pregnancy doesn’t occur. If the sperms are only produced at low levels or cannot swim well they are unlikely to make it to the egg and pregnancy is unlikely to occur. There are also many other reasons why a couple may not achieve a pregnancy. There IVF is a treatment that brings eggs and sperm together in the laboratory and encourages fertilisation to happen by providing a nourishing environment.
IVF bypasses several of the natural processes of conception in the human body such as:
IVF can also control the complex process of a sperm entering and fertilising an egg.It provides a nourishing environment as the fertilized egg develops into an embryo. The last step of IVF is to gently transfer the embryo or embryos back inside the womb where they would have been at that time had all been working as usual in the body.
 GETTING READY
GETTING READY
Once you have decided to have an IVF cycle, the first step is getting your body ready. We advise all women to start taking folic acid (minimum dose 0.4mg/day) or to take a multivitamin supplement that contains folic acid. Sometimes a medication such as the birth control pill or a monthly injection will be given to you to prepare your ovaries and womb for your treatment. The results of all your screening blood tests need to be available at this point.
A human egg is microscopic and cannot be seen with the human eye. Just to give you an idea how small and delicate they are, up to 50 eggs could balance on the tip of a pin. They require carefully controlled environmental conditions such as warm temperatures and the right gases and nutrients.
 PREPARING YOUR EGGS
PREPARING YOUR EGGS
In a woman’s natural cycle one egg grows a month. To give you a better chance of getting pregnant more eggs than this will help. To help your ovaries produce more than one egg a fertility drug (called FSH hormone) is taken by injection every day for between 8-14 days. This is carefully monitored by ultrasound scans and blood tests every few days.
Often a second drug (called Cetrotide) is needed for the last few days to prevent any eggs from being released and lost inside the woman’s body. After 8-14 days your eggs will be nicely grown and ready to be collected. At this point a special injection is given to mature your eggs so that they can be collected 34 - 36 hours later.
 COLLECTING YOUR EGGS
COLLECTING YOUR EGGS
Eggs are collected by passing a needle through the wall of the vagina into the ovary guided by an ultrasound scan. It does not require surgery and is a minor procedure which takes around 30 minutes. The eggs will be collected into the needle one by one, and placed in an incubator in the fertility laboratory by the embryologist.
For the egg collection our anaesthetic doctor will give you pain killing drugs so that you are comfortable. Most women sleep through the procedure or say that they feel very little. We will need you to stay in the hospital for 3-4 hours after your egg collection until you are well enough to go home. Because of the drugs that you will have been given, you will not be able to work for the day and should not drive afterwards or sign any legal documents.
 PREPARING THE SPERM
PREPARING THE SPERM
The day that the eggs are collected, the male partner needs to produce a sperm sample. If a donor sperm sample is being used this will be thawed. The sperm will be washed and carefully prepared so that the healthiest sperm are placed around the egg. The eggs and sperm are then placed in an incubator and left overnight to allow the natural process of the best sperm getting into the egg and fertilising it. If the sperm are low in numbers then they will have a low chance of getting into the egg on their own and ICSI or sperm injection will be a better option to give the best chance of fertilisation.
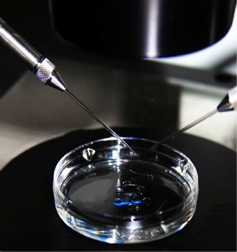
What is ICSI? ICSI (pronounced ick-see) or Intra-Cytoplasmic Sperm Injection involves injecting a single sperm into the centre of an egg. ICSI was one of the biggest advances in fertility treatment after IVF itself and has been in routine practice around the world for over twenty years. After the egg collection procedure, the eggs are prepared and examined by the embryologist in the IVF lab to check they are healthy and mature and will be suitable for sperm injection. Often 20-30% of a woman’s eggs are not healthy or mature.
In the IVF laboratory single sperm with the best shape (morphology) and swimming-ability (motility) is chosen by careful analysis of all the sperm under a microscope. The chosen sperm is gently sucked up inside a very thin glass needle. This needle is thinner than a human hair. The embryologist performs the ICSI injection using a special microscope. The pipette is positioned at the correct place ready for injection into the egg. The egg is held steady in a robotic holding pipette. The pipette pierces the outside of the egg and the inner membrane. Once the embryologist can see that the pipette is inside the egg, the sperm is injected gently into the centre of the egg and the pipette is carefully withdrawn.
The injected eggs are placed in an incubator and checked the next morning to see if they have fertilised. Usually 60-70% of injected eggs will fertilise although there is a small chance that none will fertilise (3.4%). Fertilised eggs (embryos) are then grown for a few more days in the IVF lab and watched carefully to see how they are developing. The best one two or three embryos are then chosen to be transferred back into the womb in the hope that a pregnancy will occur. Any remaining good quality embryos can be frozen and stored for future use.
REPLACING THE EMBRYOS INSIDE THE WOMB
Two to six days after the eggs have fertilised, the healthiest embryo or embryos are selected to be put back into the woman's womb. This embryo transfer procedure is not painful and takes 10-15 minutes. It feels very like having a cervical PAP smear done.
The number of embryos to be placed inside the womb will be carefully decided by you along with your doctor and the embryologist. If suitable, remaining embryos can be frozen in case you have further IVF treatment. After the embryo transfer it will be 9-12 days before you can find out whether your IVF cycle was a successful one by having a pregnancy test.
Just like human eggs, human embryos are very delicate and so small that they cannot be seen with the human eye. Many embryos would fit on the tip of a pin. They require carefully controlled environmental conditions such as warm temperatures and the right gases and nutrients. They start as one cell and will eventually grow into the billions of cells that make up a human being. Your embryos are placed back inside your womb anywhere between the two cell stage (day 2 of their life) or the blastocyst stage on day 5 or 6 where they are now several hundred cells.
What is an embryologist?
An embryologist is a scientist (and sometimes a doctor) who is an expert in the fertility laboratory. Embryologists ensure the eggs are given the right environment to thrive in the IVF lab, prepare the sperm and where needed select the best sperm and inject it into an egg (ICSI). After egg collection the eggs and sperm are mixed and left to fertilise overnight. When the sperm quality is suboptimal the sperm are injected into the egg by ICSI. The next day the embryologist checks to see how many eggs have fertilised. Those that have fertilised (now called embryos) are watched carefully for another 1-4 days as they develop.
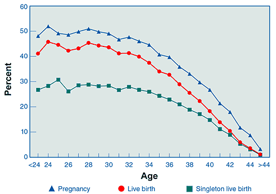 Percentages of ART Cycles Using Fresh Nondonor Eggs or Embryos That Resulted in Pregnancies, Live Births, by Age of Woman, *2010[/caption]
Every year around the world thousands of babies are born after IVF treatment. However IVF treatment certainly cannot guarantee a pregnancy.
Your chance of conceiving with IVF depends on several things. IVF is more likely to be successful when the woman is below the age of 35 years or a couple have been suffering with infertility for a short period of time (less than five years).
Trinidad IVF & Fertility Centre Success rates for 2014-2016
Fertilisation rate is the percentage of mature eggs that fertilise out of all that were collected.
Percentages of ART Cycles Using Fresh Nondonor Eggs or Embryos That Resulted in Pregnancies, Live Births, by Age of Woman, *2010[/caption]
Every year around the world thousands of babies are born after IVF treatment. However IVF treatment certainly cannot guarantee a pregnancy.
Your chance of conceiving with IVF depends on several things. IVF is more likely to be successful when the woman is below the age of 35 years or a couple have been suffering with infertility for a short period of time (less than five years).
Trinidad IVF & Fertility Centre Success rates for 2014-2016
Fertilisation rate is the percentage of mature eggs that fertilise out of all that were collected.
|
2014 - 2016 |
||||
|
Age group |
<35 |
35-37 |
38-40 |
>40 |
|
Positive pregnancy test |
46% |
50% |
50% |
14% |
|
Live birth |
33% |
34% |
27% |
3% |
|
Fertilization rate |
62% |
|||
|
Average # Embryos Transferred |
1.7 |
|||
|
Twin Rate |
4.7% |
|||
|
Higher multiple pregnancy rate |
0% |
|||
IVF is usually a very safe procedure, however like all medical treatments, there are some risks. You may experience a mild reaction to some of the fertility drugs we use including hot flushes, nausea, feeling down or irritable, headaches or restlessness and bloating. Having a multiple birth (twins, triplets or more) is the single greatest health risk associated with fertility treatment. This is why many countries have now imposed restrictions on the number of embryos that a clinic can transfer during IVF. Multiple births carry risks to both the health of the mother and to the health of the unborn babies. The babies are more likely to miscarry, to be premature and have disabilities or cerebral palsy. For this reason we carefully guide you to decide how many embryos should be placed inside your womb. IVF can also result in an ectopic pregnancy. This is when an embryo develops in your fallopian tube rather than in the womb, and can happen in a natural pregnancy or when you have become pregnant through fertility treatment. Rarely in more fertile women going through IVF the ovaries can over respond leading to a condition called ovarian hyperstimulation syndrome (OHSS).
 1. Egg damage. On inserting the sperm into the egg using there is small risk of damaging the egg. An average of 92% of all injected eggs survive the procedure.
2. Fetal abnormalities. Children born after ICSI treatment have been closely followed up in many countries and the data so far has been reassuring that there are no significant increases in birth defects or other common problems. One or two countries have noticed a slightly higher rate of some rare genetic and developmental defects in a very small number of children born after ICSI.
However, these problems may actually have been caused by the underlying infertility problems, rather than the ICSI treatment. At the moment we do not studies are collecting more information.
3. Boy children may inherit a genetic infertility problem. It is possible a boy baby conceived as a result of ICSI may inherit his father’s infertility (if it had a genetic cause).
It is too early to know if this is the case, as the oldest boys born from ICSI are still in their early teens. However if the father’s infertility problem had a genetic cause then this is likely to be passed on to any boy children born with ICSI. For this reason couples should consider undergoing genetic tests before going ahead with ICSI, to see if the male carries any genetic causes for infertility that can be detected at the present time.
1. Egg damage. On inserting the sperm into the egg using there is small risk of damaging the egg. An average of 92% of all injected eggs survive the procedure.
2. Fetal abnormalities. Children born after ICSI treatment have been closely followed up in many countries and the data so far has been reassuring that there are no significant increases in birth defects or other common problems. One or two countries have noticed a slightly higher rate of some rare genetic and developmental defects in a very small number of children born after ICSI.
However, these problems may actually have been caused by the underlying infertility problems, rather than the ICSI treatment. At the moment we do not studies are collecting more information.
3. Boy children may inherit a genetic infertility problem. It is possible a boy baby conceived as a result of ICSI may inherit his father’s infertility (if it had a genetic cause).
It is too early to know if this is the case, as the oldest boys born from ICSI are still in their early teens. However if the father’s infertility problem had a genetic cause then this is likely to be passed on to any boy children born with ICSI. For this reason couples should consider undergoing genetic tests before going ahead with ICSI, to see if the male carries any genetic causes for infertility that can be detected at the present time. This is the website for the HFEA, the UK government’s impartial independent fertility clinic regulator.